Download Nevada EMS
Download Nevada EMS
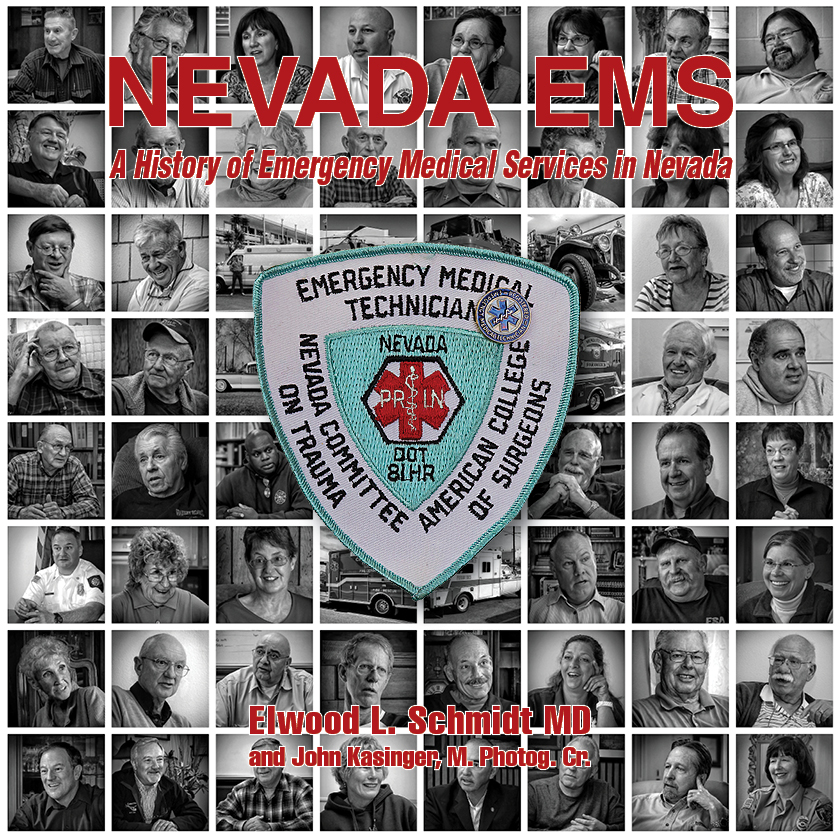
My first book Nevada EMS – A History of Emergency Medical Services in Nevada is now available as a free downloadable PDF file. Get your copy here.
The file is about 159MB, so please be patient as it downloads.
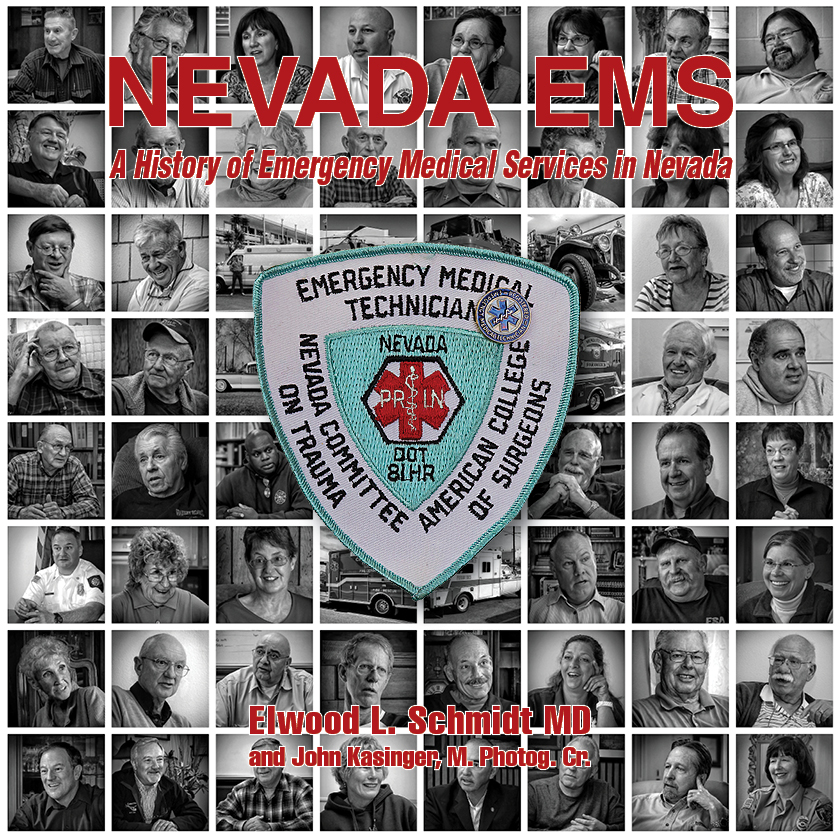
My first book Nevada EMS – A History of Emergency Medical Services in Nevada is now available as a free downloadable PDF file. Get your copy here.
The file is about 159MB, so please be patient as it downloads.
Those words can make the physician shudder. In the years before 1970, approximately, the words translated to, “Do all the tests and treatments you think might help mom get over her condition, or at least make her comfortable.”
In the mid to late 1960’s it became apparent that people were dying in the hospital, at home, or on the street with functional hearts that happened to beat irregularly. If untreated that person proceeded to death. It was found that in hospital or out, a person’s circulation could be maintained to the brain and heart and other vital organs until a hospital team could convert the heart beat to a regular rhythm. Many people have been able to live normal lives after a near death experience.
Some unfortunate rulings by state attorney general in Mass. and NY made failure to do a full resuscitation effort on all dying patients a criminal offense. As a result, physicians often feel, are, obligated to perform chest compressions to perfuse blood while intubating and breathing for the patient and administering electric shocks to the heart and injecting a multitude of drugs in an all-out effort to prevent death that is inevitable from other than cardiac causes. Only after all these steps to the “Modern American Hospital Death Dance” have been completed is the person allowed to be dead, for good and certain dead.
“Do Everything You Can for Mom-Do Everything”
We all need to be certain what everything is. We need to let our families know what our hopes and expectations are when death is expected. We need to have executed a medical power of attorney and/or completed an advance directive form. When we have done those things, then we will have done everything for Mom (and Dad of course.)
I continue, “ You know something about diabetes because of your family history. You are going to learn a lot more about diabetes as its control is up to you. You are going to see the dietitian with your husband so he also has some understanding of your dietary needs. You are going to see the diabetic educator at the hospital and learn other important things about taking care of your diabetes. The four most important things you will learn is proper diet, regular exercise, regular exercise, and proper diet.”
I deliver these words with passion. My eyes are intent on my patient. I am animated because I want her to know how important her participation in the care of her diabetes is to successful treatment. I sit back and ask her, “Any questions?”
Her reply, “Can’t you just give me a pill for it?”
In one of my practice locations I became friendly with an accountant. His wife, his mother, his mother-in-law, and his father-in-law were all my patients. I thought I knew the family pretty well, but there were hidden secrets.
On the occasion of his mother’s periodic check up she suddenly made me aware of a problem. “You know Richard has a temper. You might not know that when he blows up periodically he hits Susan and has hurt her quite a bit. I’ve talked to him but it doesn’t do any good. He thinks the world of you, and if you talked to him he might change.”
I masked my shock at this revelation and told her I would try to change the behavior. How I would do this would challenge me as no one likes to be confronted with abhorrent behavior directly.
Richard and I had lunch together periodically and I approached the problem obliquely.
I arrived at the lunch place late and showing my agitation. “ I don’t usually see you like this. What’ got you so upset ?” he asked.
“ Well I saw this woman this morning and she had bruises on her chest and legs and was really agitated and crying. When I asked her how she got the bruises she finally told me that her husband would beat on her periodically, and she was scared to defend herself. I knew her husband was in the waiting room so I went out there and asked him to come to my office. When he came him into the office I slammed the door and got in his face and told him what miserable piece of crap I thought he was and that I would personally beat his ass if he did that again as well as report him to the police. I don’t know if I could whip him but he saw how P. O.ed I was and he folded up.”
“Do I know this guy?” my friend asked.
“You might, but I’m not about to break patient confidentiality. It just makes me so mad that a big man will beat on a woman like that. You know I have had my share of aggravation from women and felt like hurting them, but that just seems so despicable to me. I just can’t see a big man beating on a woman. It’s disgusting.”
The conversation soon moved on to other topics and we left in our usual state of pleasure at the conversation on gossip in the community and the world.
Maybe three months or so later I saw his mother. “You really must have told Richard off. He hasn’t hit Susan since we talked and he’s treating her nicer than he ever has before. Thank you. You must have really laid the law down to him.”
Over the ensuing years I never heard another word about abuse from Richard and I wasn’t about to tell anybody about my subterfuge, until now.
(Originally published by Nevada Humanities, www.nevadahumanities.org, on July 12, 2021.)
Each evening as I sit at the kitchen table my view is of the Virginia Range. For 26 years I have watched the light and shadows on the ridges and gullies of the Virginias sharpen, soften, then fade into darkness and change with the seasons.
The scene has always been pleasing to me and a soothing way to mark the end of a day. I know the sun will arise behind these mountains each morning, putting them in silhouette. Then full light, and clouds willing, to the play of light and shadow I enjoy each evening.
I practiced medicine for 50+ years. I was a hospice medical director for 15 of those years. I attended many people as they approached the end of their lives. Many people noted how much sharper their appreciation of the small scenes of life had become. I read in stories—short and long—of a similar sense among other people. I thought I appreciated these scenes—the daffodils blooming, the greening of the grass, the smell of the hyacinths and the changes that each season brings to us.
My 89th year is flowing along with a twitch here, a twinge there, a bump in the chest again and again, and my sense of my own mortality grows stronger. My appreciation of these mundane scenes has gone from an intellectual aesthetic appreciation to one of deep feeling in my own essence.
Perhaps this is because of the heightened sense of mortality brought about by the COVID-19 pandemic with the daily headlines of death; perhaps it is the conversation with a dear friend whose health is rapidly deteriorating, and she sees the end of life racing toward her. Whatever the reason it is pleasing to embrace this heightened awareness into my life.
My wish is that everyone can have the opportunity to reach a similar state for themselves. An evening view of the Virginias in Reno, or the Red Rocks in Las Vegas, are a great aide to achieving that feeling.